CALCIPOTRIOL AND 5-FLUOROURACIL (5-FU)

Calcipotriol and 5 Fluorouracil (5-FU)
Cytokines are cell signalling molecules that aid cell to cell communication in immune responses and stimulate cells to move toward sites of inflammation.
Thymic stromal lymphopoeitin (TSLP) is an epithelium-derived cytokine that induces a robust anti-tumour immunity in barrier-defective skin. Calcipotriol (Daivonex), an ointment most commonly used in psoriasis, is a topical TSLP inducer.
5-FU cream (Efudix) is an anti-metabolite that blocks the growth of abnormal cells and is frequently used to treat pre-cancerous solar keratoses. But there are major disadvantages including the long treatment/healing duration (1-2 months) and the severity of the side effects - pain, irritation, burning, crusting, photosensitivity.
Efudix cream and Calcipotriol ointment used together (FU/Cal) twice daily for a 4-day treatment of solar keratoses has been shown to be more effective than using Efudix alone! The short treatment duration and minimal side-effect profile in a trial conducted at Washington University and Massachusetts General Hospital highlight the advantages of this combined therapy which resulted in a specific induction of CD4+ ’T helper cell’ immune response against solar keratoses. These are considered helper cells because they do not neutralise but trigger the body’s immune responses.
Halo Graft

Halo graft
A skin graft is transplantation of skin from one location to another on the same individual and has been used in patients since 1869.
A split skin graft (SSG) involves a very thin shaving of skin including epidermis and a small portion of dermis leaving behind the enough dermis for the donor site to heal by reepithelialisation. A SSG is more likely to survive in areas with less vascularity such as periosteum and peritenon and is graft of choice for the shin.
Dr Sharad Paul, a NZ doctor, described a type of SSG which can be done under local anaesthesia in only one area (instead of different donor and recipient sites), decreases healing times and donor site pain… the Halo Graft.
The central defect is where the lesion is excised, and the ‘halo’ or annulus around the circular excision margins is where the donor site shavings are harvested for the SSG. The wound is usually completely healed in 2-3 weeks. Ingenious!
SUBUNGUAL AND ACRAL LENTIGINOUS MELANOMA

Subungual and Acral Lentiginous Melanoma
Acral lentiginous melanoma (ALM) arise on the palms, soles or beneath the nail (subungual melanoma). It is a form of malignant melanoma (MM) characterised by its site of origin. In the past, subungual melanoma (SUM) have always been considered a subtype of ALM. SUM is more common on the feet than hands. Although ALM is a relatively rare type of MM (1-3%), it is the most common subtype of MM in darker skinned people. Bob Marley, black reggae musician, died of an SUM under his toenail.
The proximal nail fold is part of the acral skin which eventually becomes the nail matrix. This is why SUM is naturally considered a subtype of ALM. Melanocytes are present in the nail matrix, but in fewer numbers than in normal skin, and in even fewer numbers in Caucasians. It is thought that these melanocytes do not produce melanin and are inactive.
However, a recent study in the Melanoma Research journal, showed that SUM are perhaps indeed a separate entity to ALM. Compared to patients with ALM, SUM were younger at diagnosis, had higher prevalence of primary MM of the hand, had more frequent reports of previous trauma at the tumour site, and were deeper at diagnosis correlating with an increased frequency of metastases. Interestingly, KIT and KRAS mutations were predominantly found in SUM whereas BRAF and NRAS mutations occurred almost exclusively in ALM.
Immunotherapy
Immunotherapy
The American Journal of Public Health published a study from New York University that showed between 1986 and 2013 new malignant melanoma (MM) cases more than doubled and mortality rates increased by nearly 10%. Not great numbers.
However, from 2013-2016, overall MM mortality decreased by nearly 20% with reduction in deaths seen in every age group. This is the largest and most sustained improvement in mortality ever observed!
Enter the new targeted therapies (-nib’s) and immunotherapies (-mab’s) which became available since 2011 and is credited with the successful results treating metastatic MM.
Immune checkpoint inhibitors encourage the patient’s own immune system to attack the MM cells (eg ipilimumab, pembrolizumab, nivolumab). Targeted therapies are specifically targeted to the patient’s tumour and more specifically at BRAF and MEK proteins known to be part of the cell signalling pathway that drives growth of MM cells. Examples of BRAF inhibitors (vemurafenib, dabrafenib, encorafenib) and MEK inhibitors (trametinib, cobimetinib, binimetinib). In about half of all MM, the BRAF protein is genetically mutated so it can no longer regulate normal cell multiplication and grow out of control. MEK is an enzyme that works with BRAF to regulate cell growth.
Sunblock

Sunblock
Primary prevention through sun protection was shown to be the most effective with 44% reduction in the incidence of MM, 39% reduction in projected MM deaths, 27% fewer excisions of keratinocyte cancer (BCC and SCC), 22% reduction in societal costs.
More evidence to the importance of sun protective measures and that you continue to slip (on a shirt), slop (on sunscreen), slap (on a hat), seek (shade) and slide (on sunglasses).
Risk Factors for SCC Recurrence
Perineural invasion in dSCC
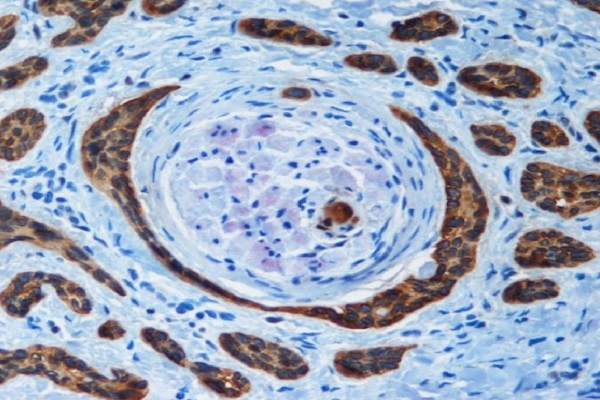
The desmoplastic type of squamous cell carcinoma (dSCC) is one that has fine branches surrounded by a desmoplastic stroma or connective tissue. dSCC accounts for just under 10% of all cutaneous SCC and is clinically indistinguishable so only diagnosed on histological examination.
Perineurial invasion (PNI) of the cancer in the space surrounding a nerve only occurs in dSCC which represents about 15% of all SCC. Patients with dSCC and PNI have significantly more lymph node metastases, local recurrences and tumour specific mortality than non-desmoplastic SCC or dSCC without PNI.
Apart from desmoplasia and PNI, significant independent factors for SCC recurrence include poor differentiation, thickness >6mm, tumour horizontal size >20mm and immunosuppression.
